Allergy & Immunology
Medical billing for Allergy, Immunology and ENT professionals is highly complex and requires trained professionals to help ensure accurate and timely reimbursement.
Among individual insurance companies, allergy testing and serum reimbursements are treated differently, requiring increased vigilance to billing and payment changes. If your practice accepts Medicare, there is a completely different set of rules governing serum billing and mistakes in the billing process can result in heavy fines from CMS.
Learn more

Dermatology
Medical billing for dermatology professionals is vastly complex and requires a highly trained staff to help ensure accurate and timely reimbursement. From simple lesion removals to complex skin grafts, dermatology billers face unique challenges in the struggle to keep practice revenue flowing. From ensuring every allergen is counted to avoiding scratch and patch test underpayments, our core team of medical billing specialists is well-versed in ICD-9, CPT and HCPCS coding systems specific to dermatology, and have high proficiency in medical terminology, skin disease processes and pharmacology.
Learn moreAnesthesiology
Anesthesia medical billing differs from all other medical specialties – time unit calculations, anesthesia specific modifiers as well as concurrency and medical direction nuances frequently leave practices underqualified and understaffed to bill effectively. These complexities combined with declining payments, increasing patient responsibility and operational costs demand efficient and accurate billing to maximize reimbursement.
For over 30 years, PGM has provided anesthesiologist and pain management practices medical billing solutions that maximize reimbursement, reduce costs and streamline practice operations.
Learn more

Cardiology
Recent changes to coding and billing regulations have led to considerable fee reductions in cardiology billing over the last several years. While the average Medicare fee increased by 1.1%, Medicare fees for cardiology have declined by nearly 2% year over year. Changes in the treatment of in-office imaging, echo services like Doppler and color flow, follow-up on implanted devices and external devices including new codes for interrogation and reprogramming of ICM and ICD devices often lead to billing errors and reduced payment. If your cardiology billing department is not fully aware of these ongoing changes and the necessary response methods, you may see a significant negative impact on your practice's bottom line.
Learn moreYou focus on patients.
Let us worry about your medical billing.
Chiropractic
A recent study by the Department of Health and Human Services found that Medicare inappropriately paid $178 Million for chiropractic billing claims on services determined to be miscoded. Additionally, CMS estimates that over 83% of chiropractic claims failed to meet one or more documentation requirements. Coding and medical billing errors such as the misuse of the acute treatment (AT) modifier to identify services, treatment or improper documentation frequently lead to denied and misadjudicated claims. Accuracy is essential for correct reimbursement and will help protect chiropractors from both malpractice and litigation.
Learn more
ASC Billing
Did you know that for Medicare patients, ASCs should report bilateral procedures as a single unit on two separate lines or with "2" in the units field on one line in order for both procedures to be paid? CMS will not recognize the use of the -50 modifier for ASC billing payment purposes and may result in incorrect payment to ASCs. The multiple procedure reduction of 50 percent will apply to all bilateral procedures subject to multiple procedure discounting.
Learn moreEmergency Medicine
Emergency Medicine presents a unique set of challenges for medical billing. High-volume, and fast paced, Emergency Medicine encompasses elements of Primary Care, Diagnostic Testing, Evaluation and Management services as well as Trauma services. Medical billing for emergency medicine includes multi code surgical procedures as well as diagnostic testing. Documentation must be precise and accurate coding and billing is critical. Recent changes to V-codes, late effects, traumatic seizures, and pain diagnosis are just some of the challenges medical billers face.
Learn more

Gastroenterology
Did you know that billing for a colonoscopy requires noting advancement beyond the splenic flexure? Otherwise, documentation will only support a sigmoidoscopy.
Accurate medical billing and coding for gastroenterology is challenging and requires a high level of knowledge to ensure maximum reimbursement. These challenges include billing for colorectal cancer screenings vs. colonoscopies, motility and GI function studies, documenting proper levels of evaluation and management services, category III codes for treatment of GERD and applying the use of modifiers -51, -59 and -26.
Learn moreOur medical billing service is a hassle-free business
solution for physician practices of any size.
Mental Health
Mental health services comprise one of the widest scopes in healthcare, encompassing patients of all ages, socioeconomic groups as well as services provided. Practitioners administer care for patients with all types of acute and chronic, mental and social health issues, including those categorized as serious mental illness. Services are often rendered in multiple facilities and locations and coverage for diagnosis and treatment vary widely by both state and payor guidelines.
Medical billing for mental health professionals is complex and time consuming, requiring trained staff to ensure accurate and timely reimbursement.
Learn more

Nephrology
Did you know reimbursement for dialysis session supervision requires the attending physicians to be present during a procedure? Are you billing a 90935 instead of a 90937?
Nephrology medical billing is highly complex and requires dedicated resources to manage, understand and navigate ever-changing federal guidelines and insurance requirements. Inadequate and incorrect documentation often result in costly errors, denied or misadjuticated claims, and on occasion can expose a practice to RAC audits and legal proceedings. It is no surprise that the average nephrology practice has experienced a 9% reduction in reimbursement over the past five years.
Learn moreOncology
Did you know that Medicare pays for chemotherapy administration only if the oncologist gives the patient a cancer diagnosis?
Oncology billing practices face reimbursement reductions, frequent coding changes, evolving compliance rules and payor ignorance regarding the latest technology. Unprofitable chemo & non-chemo drug reimbursement, negative payment margin on drug purchases and complex coding and billing requirements seriously erode practice revenue. Coding and medical billing errors such as the misuse of modifiers to identify services, treatment or improper documentation frequently lead to denied and misadjudicated claims.
Learn more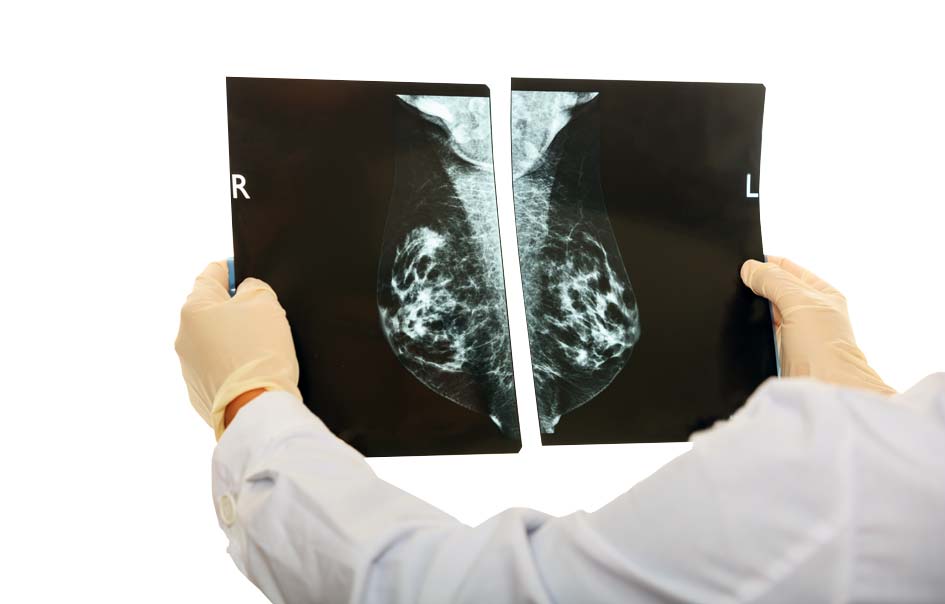

Orthopedic
Did you know that pain pump insertions provided for post-op pain relief are only billable when they are performed by a physician other than the orthopedic surgeon?
Approximately 35% of all orthopedic surgery claims are processed incorrectly by commercial carriers. To make matters worse, over 25% of all medical claims are rejected, of which 15% are never resubmitted. With the billions of claims filed each year, it is estimated that over $65 billion of orthopedic billing revenue is left on the table.
Learn morePGM's full range of practice management solutions
will liberate your staff of tedious physician billing
and remittance tasks
Pain Management
Anesthesia billing differs from all other medical specialties – time unit calculations, anesthesia specific modifiers as well as concurrency and medical direction nuances frequently leave practices underqualified and understaffed to bill effectively. These complexities combined with declining payments, increasing patient responsibility and operational costs demand efficient and accurate billing to maximize reimbursement.
For over 30 years, PGM has provided anesthesiologist and pain management practices medical billing solutions that maximize reimbursement, reduce costs and streamline practice operations.
Learn more

Primary Care
Primary care involves the widest scope in healthcare, including patients of all ages, socioeconomic groups as well as services provided. Physicians provide care for patients with all types of acute and chronic physical, mental and social health issues, including multiple chronic diseases. As a result, a primary care practitioner must possess a wide breadth of knowledge in a multitude of areas. Whether the physician is administering vaccinations, reporting E/M services, treating a cold or providing smoking cessation education, you need to be well-versed in primary care billing for virtually any condition.
Learn moreUrology
Did you know most urology practices leave 10-20% (conservatively) in reimbursements on the table due to poor process, staff skill levels, lack of technology and ineffective management?
Urology medical billing is highly complex and ever changing. Confronting declining payments, increasing patient responsibility and increased operational costs requires efficient and accurate medical billing procedures. Payor differences in the treatment of infusion immunotherapy, postoperative complications, urodynamics, etc., leave practices under qualified and frequently understaffed to bill effectively.
Learn more