




balancing the role between physician and business person.
Physician practices all across America face similar challenges. With decreasing reimbursements and increasing denial rates, practices are seeing a serious impact on their bottom line. In addition, as insurance carrier and HIPAA requirements change, physicians are dedicating more of their time and resources to administrative tasks and red tape.
To meet these challenges, you need a partner who understands the complexities of healthcare management. Since 1981, PGM has been providing practice management and billing services to physicians and healthcare facilities across the country. Our specialized medical billing service is focused on helping physicians not only get paid more, but get paid faster.
PGM’s technology plus service approach to practice management maximizes the reimbursement process and helps streamline practice operations. You will see an improvement in day to day collections and cash flow and gain increased insight into practice performance. The end result? Enhanced profitability and more time to deliver the highest level of patient care.
Have the most time-consuming work done for you.
Our complete practice management solution eliminates all charge entry, claim submission and follow-up, payment posting, advanced claim scrubbing to minimize denials, and much more.
• Claims submission and tracking helping to ensure timely payment.
• Remittance advice posting, including EOB scanning and payment verification.
• New payer rule development helping to monitor changes and keep payments on track.
• Extensive follow-up and appeals process where nothing gets left behind.
• No-hassle, web based software that is easy to use, learn and implement.
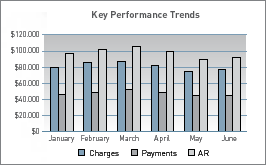
• Fully customizable reports available 24/7 in real-time, providing in-depth visibility into practice performance and trends.
• A global dictionary of insurance package information, ensuring proper payer enrollment.
• Periodic account reviews where we examine payer successes and opportunities for improvement.

your time to payment with PGM.
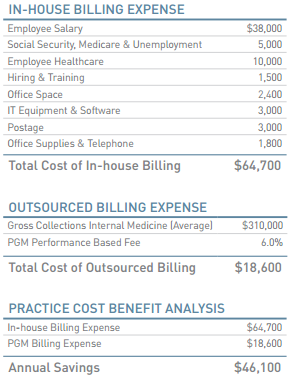
Cost Effective
We get paid only once you get paid—PGM is 100% performance driven. With PGM, your costs are directly proportionate to your actual income. There are no dedicated staffing or administrative expenses related to in-house billing. In addition, there are no initial start up costs, no hidden or ongoing expenses, and no costly investments in hardware and software.
Improved Performance
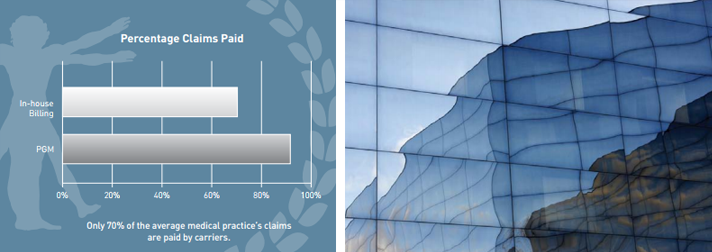
Our comprehensive service is focused on maximizing your collections, getting you paid more and paid faster. Our clients typically see a 25–30% increase in net collections within six months. Our advanced claim reviewer detects billing errors prior to entry, dramatically reducing denial rates. We aggressively follow-up and appeal denied and miss-adjudicated claims. In addition, we assume full responsibility for responding to all inquiries from patients and third party carriers, helping to increase your bottom line.
- Improve
Your collection rate - Shorten
Your reimbursement cycle - Reduce
Your accounts receivable - Decrease
The rate of lost and denied claims - Gain
Improved insight into your practice’s financial performance

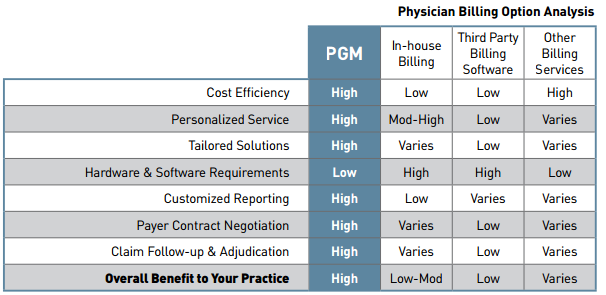
Tailored to Your Needs
PGM understands that all medical practices are not the same. We provide physicians with a solution tailor made to the individual needs of any practice. From full service medical billing, to extending to you our proprietary software (where you retain full control), PGM offers the complete range of practice management services. We will work with you and your staff to design a program that best fits the needs of your practice.
U.S. Owned and Operated – At PGM we pride ourselves in our commitment to our U.S. based operations. It is our firm belief that the benefits of knowledgeable, experienced and accessible U.S.- based employees far outweigh any cost savings associated with off-shore practices.
Personalized Assistance.
Our staff is 100% committed to serving you. All of our clients are assigned their own designated Account Executive, giving the security and comfort of working with a representative who is uniquely familiar with your practice. From guiding you through the implementation process to frequent performance reviews and updates, our staff is there with you every step of the way.

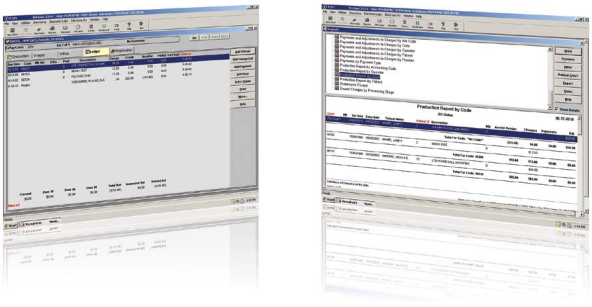
Access to real-time, in-depth visibility and reporting.
Understanding your practice’s financial performance can be challenging. With data buried in patient charts, spreadsheets and antiquated systems, gathering the information necessary to optimize operations and plan for the future is often difficult and time consuming.
To help meet this challenge, PGM provides you with advanced financial and practice analysis tools, specifically designed to give enhanced visibility of your operations at the click of a button.
PGM reporting is user friendly and grants instant access to data so you can instantly track performance and make qualified decisions. Qualitative assessment becomes easier, because you can review everything from which payers reimburse, and at what rates to which business lines are most successful.
Selected Finacnial Reports
- Summary Report:
Overview of all charges, payments, and adjustments. - Accounts Receivable Report:
Up to the minute, detailed or summarized aged receivable information that will give you 100% visibility over your uncollected claims. - Revenue and Production Reports:
Allows you to analyze your procedures by code, giving you better insight into how you allocate your time. - Payment and Charge Reports:
List of payments received and charges submitted, helping you to categorize payments and charges by multiple variables including: location, physician, insurance carrier and more.

Selected Practice Analysis Reports
- Frequency of Procedure/Diagnosis:
Examine the most common procedure, diagnosis code, and other information recorded within you practice. - Payment Reimbursement:
Analyze the payment history by insurance carrier, helping you to determine if contracted carriers are meeting their negotiated fee schedules. - Denial Report:
Review claim denials by insurance carrier, helping you to identify areas of improvement and carrier abuses.
Selected Finacnial Reports
Benefit from no-hassle software, easy implementation, and automatic updates. From any internet enabled computer or mobile device, you can analyze payments by carrier, provider, location, procedure, diagnosis, timeframe and much, much more.
There are currently several hundred standard reports to choose from, as well as customizable reports that replace the static reports generated by typical billing software. Many of PGM’s reports have been recommended and modified by PGM clients to provide the necessary information relevant to you.
With PGM reporting, you get clearer visibility into practice operations and claims’ status, all updated in real time. Reporting capabilities are focused on increasing your bottom line and giving revenue control back to your practice.

The PGM Process
- Patient and charge data exports are collected from your office daily.
- Patient demographics and charges are keyed by our staff or electronically transferred though our EMR/billing interface.
- Medical claims process software is used to scrub claims for errors and submit claims electronically.
- Insurance payments are received via paper or electronic remittance advices. Payments can be received at either the practice location or at PGM.
- Payments are reviewed, line-item posted into the system, compared against fee schedules and then balanced. This performed at the time of payment posting to help ensure correct reimbursement.
- Patient balances are billed and should the patient fail to respond, a letter and/or call sequence is initiated to obtain payment. It is important to note that patients are provided with a toll-free number to call with any questions about their bill.
- AR aging reports will be carefully processed and sent for your appraisal.
- Once an outstanding claim has been identified as past due, the PGM’s system alerts our Reimbursement Specialists who then review the history and follow-up on the claim accordingly
- Reports are sent on a weekly/monthly basis and are available online 24/7 for client review.
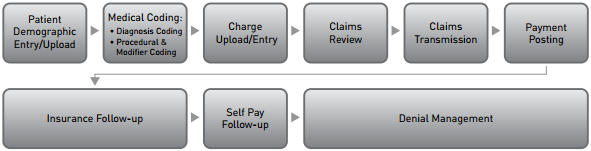
PGM’s practice management solutions allow your practice to eliminate all charge entry and patient demographic updates, as well as payment posting. A dedicated team of Account Representatives will enter all charges, perform claims scrubbing, post payments, bill patients, and most importantly, follow-up on all denials.
- Electronic and Paper Claims Filing
PGM manages all data entry, claims and claims tracking for you. We have the capability to transmit claims electronically to thousands of insurance carriers. - Claim Follow-up
At PGM, claim follow-up is a priority. Our staff regularly follows-up on the progress of your claims to make sure you are receiving prompt, correct payments. - Advanced Claims Review System
PGM’s advanced claims scrubber identifies and corrects errors and omissions before claims are submitted. The results are reduced denials and faster reimbursement. - EMR Compatibility
Our software has the capability to integrate with any existing EMR system.
- Patient Invoicing, Collection and Inquiries
PGM manages all data entry, claims and claims tracking for you. We have the capability to transmit claims electronically to thousands of insurance carriers. - Financial Reporting
PGM provides your practice with financial and practice analysis reports available in the industry today. - Custom reports can be generated at your request, and a wide range of standard reports are instantly available.
- Remote Access
We provide internet access to all of your account information, giving you direct visibility over patient data, current charges and balances, as well as financial performance. - Claim Adjudication
Only 70% of the average medical practice’s insurance claims are ever paid by carriers. PGM aggressively monitors and accesses EOBs and payments to ensure the highest possible reimbursement rate.


