PGM: The Mental Health Billing Experts
Running a successful mental health organization requires expert billing solutions that boost revenue while reducing administrative burdens. At PGM, we specialize in mental health billing services, ensuring providers receive full reimbursement while maintaining compliance with complex insurance regulations.
When you partner with PGM, one of the country’s leading mental health billing companies, you gain access to experienced billing professionals who understand the intricacies of billing for mental health services, from proper coding and payer requirements to regulatory compliance. Our dedicated team ensures accurate claim submission, denial prevention, and seamless behavioral health revenue cycle management, so you can focus on providing quality client care.
Whether your practice specializes in psychotherapy, psychiatry, or substance abuse treatment, our customized behavioral health billing solutions are designed to optimize cash flow and reduce operational costs. More mental health providers are choosing PGM due to our commitment to accuracy, transparency, and financial success.
Contact PGM today to learn how our specialized mental health billing services can help your practice thrive.

The Leading Choice for Mental Health Billing Services
Managing a successful mental health practice requires expertise not only in client care but also in navigating the complexities of mental health billing services. From coding accuracy to payer-specific requirements, the financial health of an organization depends on efficient billing for mental health services. At PGM, we specialize in streamlining the behavioral health revenue cycle management process, ensuring that providers receive maximum reimbursement while minimizing administrative burdens. Our dedicated team understands the unique challenges associated with billing for behavioral health services.
With decades of experience, PGM has built a reputation as a leader in behavioral health billing, offering tailored, scalable solutions that enhance efficiency and revenue flow. We utilize cutting-edge technology, expert billing professionals, and a proactive approach to claim management to improve clean claims, reduce denials, and drive better cash flow. Whether you’re an independent therapist, a multi-provider clinic, or a large mental health organization, our comprehensive mental health billing solutions are designed to strengthen financial performance, allowing you to increase client volume and provide high-quality care and support.
The Unique Challenges of Behavioral Health Billing
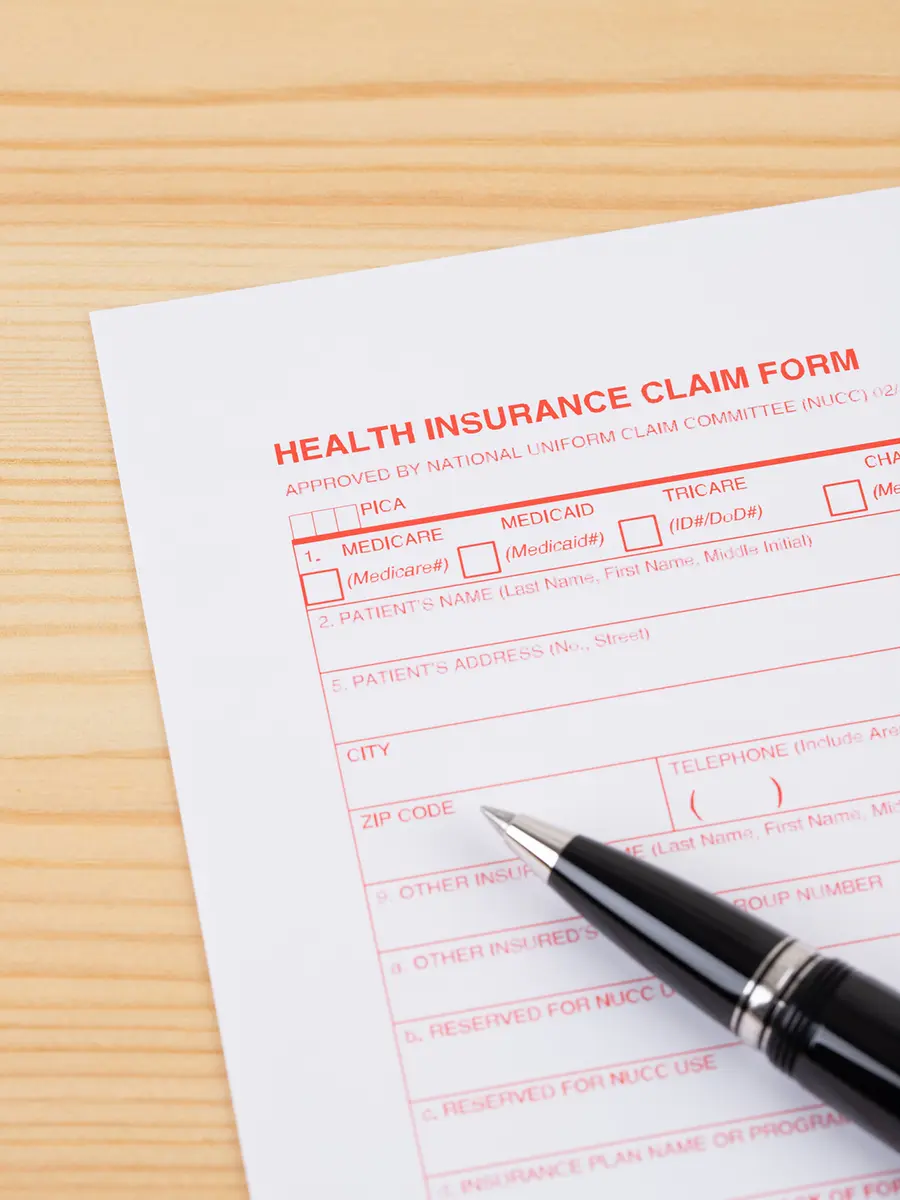
Billing services for mental health presents unique challenges due to complex payer policies, strict documentation requirements, evolving regulations, and many other challenges. Successfully managing billing for behavioral health services is essential for timely reimbursements and financial stability.
One of the primary complexities of mental health billing is navigating payer-specific rules for services like therapy, medication management, and telehealth. Each insurance company has distinct billing codes, claims requirements, coverage limitations, and reimbursement rates. For instance, some insurers require pre-authorizations for therapy sessions beyond a set limit, while others have specific time-based billing codes that impact reimbursement rates. Failure to comply with these nuances can result in denied claims, delayed payments, and even revenue loss.
For providers who accept Medicare and Medicaid, billing becomes even more complicated. Strict – and often changing – guidelines govern billing for mental health services, requiring precise documentation, coding accuracy, and adherence to reimbursement policies. Non-compliance can lead to audits, penalties, and legal risks, making expert billing support essential.
Full-Service Mental Health Billing by PGM
PGM specializes in behavioral health billing services, ensuring compliance, correct and complete reimbursements, and minimized denials. Our deep industry knowledge helps practices navigate the challenges of behavioral health billing, improving revenue cycle performance and operational efficiency.
Mental Health Services Billing
Billing for mental health services requires precise coding and documentation. Whether it’s individual therapy, group therapy, or psychiatric evaluations, PGM ensures accurate coding and submission to prevent underpayments, denials, and clawbacks.
Modifier Management
Correct application of CPT and HCPCS modifiers is crucial in billing for behavioral health services, especially for services involving multiple providers or extended sessions. PGM ensures the consistent and correct use of modifiers, helping ensure our partners receive proper reimbursement while always following the rules and regulations.
Proper Mental Health ICD-10 Code Selection
Accurate ICD-10 coding is essential for properly documenting conditions such as anxiety disorders (F41.1) or major depressive disorder (F32.9). Our certified coders stay current with the latest coding updates, which increases clean claim rates and decreases denials and delays.

What To Expect: Maximized Reimbursement and Compliance
PGM’s expert mental health billing services help practices enhance revenue, minimize errors, and maintain compliance. Our clients typically experience a 20-30% increase in collections, a 40% reduction in denials, and significant improvements in behavioral health revenue cycle management performance.
How PGM Gets the Best Results in Mental Health Billing
PGM is a leader in mental health billing services because we combine advanced technology with expert billing support to optimize revenue and minimize administrative burdens. Our dedicated team understands the complexities of billing for behavioral health services, ensuring that providers receive the reimbursements they deserve without unnecessary claim delays or denials. By implementing industry-leading technology and a proactive approach to revenue cycle management, we help practices streamline their operations while meeting ever-changing regulations.
Our success in behavioral health billing is driven by key factors, including:
-
Complete Behavioral Health Billing Services
From claim submission to full behavioral health revenue cycle management, we ensure accuracy and efficiency. -

Mental Health Billing Software Integration
Our innovative software automates billing tasks, reduces errors, and strengthens coding accuracy. -
Payer Negotiation Strategies
We work with insurers to secure optimal reimbursement rates for mental health billing. -

Personalized, Flexible Billing Solutions
Unlike generic billing providers, PGM offers customized solutions tailored to the unique needs of mental health practices. -
Regulatory Oversight
Our team stays updated on changing insurance policies to ensure compliance with Medicare, Medicaid, and private payers. -
Denial Prevention and Revenue Optimization
We proactively monitor claims, resolve denials quickly, and enhance cash flow. -

End-to-End Mental Health Revenue Cycle Management
From client eligibility verification to payment posting and financial reporting, we handle the entire revenue cycle. -
Data-Driven Analytics for Financial Optimization
Our advanced reporting tools provide actionable insights into billing performance, helping our practices identify trends, increase reimbursement rates, and improve decision-making.
PGM Revenue Cycle Management
Mental Health Billing Software Solutions
PGM offers cutting-edge billing software to streamline mental health billing services, automate processes, and reduce errors. Our system effectively integrates with EHRs, minimizing manual data entry while ensuring accurate coding and reducing claim denials. With real-time claim tracking and compliance tools, our software helps providers manage client data and navigate complex insurance rules effortlessly. Advanced reporting features also support behavioral health revenue cycle management, optimizing financial performance and reimbursements.
Proof in Numbers
With our deep expertise and extensive experience in providing mental health billing services, practices can expect increased efficiency, improved reimbursement, and a significant reduction in administrative burdens. By partnering with PGM, mental health providers gain more time to deliver quality client care, while we manage the complexities of mental health medical billing.
Why Choose PGM for Your Outsourced Mental Health Billing and Coding?
PGM specializes in mental health billing services, providing tailored solutions that streamline operations, decrease denials, and ensure accurate reimbursements. Our expert team understands the complexities of billing for mental health services, ensuring accuracy in coding, compliance with insurance regulations, and efficient claim processing. Whether you operate a solo practice or a large behavioral health facility, we offer comprehensive behavioral health revenue cycle management designed to improve cash flow and financial stability. By leveraging cutting-edge technology and proactive support, we help mental health providers minimize administrative burdens and focus on delivering quality client care. When you select PGM, you will be getting a partner recognized as one of the best behavioral health billing companies in business today.

Specialized Knowledge in Mental Health Billing Services
With decades of experience in behavioral health billing, PGM ensures providers receive maximum reimbursement while following payer policies. Our team is highly skilled in managing billing for behavioral health services, including therapy sessions, psychological assessments, medication management, and crisis interventions. We navigate complex coding requirements, insurance authorizations, and regulatory updates to prevent claim denials and revenue loss. By offering end-to-end mental health billing solutions, from eligibility verification to payment reconciliation, PGM helps practices elevate their financial performance and achieve long-term stability.
Certified Experts in Behavioral Health Billing
Our certified billing specialists stay up to date with the latest CPT, ICD-10, and HCPCS codes, ensuring compliance and reimbursement success. We have extensive experience in billing for behavioral health services, including:
- Psychotherapy (CPT 90834, 90837)
- Psychiatric diagnostic evaluations (CPT 90791, 90792)
- Group therapy (CPT 90853)
- Medication management (CPT 99212-99215)
- Telehealth mental health services (CPT 96127, 90846-90847)
Personalized Billing Solutions for Mental Health Providers
Unlike generic billing providers, PGM offers tailored mental health billing solutions designed to meet the unique needs of behavioral health practices. Our software integrates seamlessly with EHR systems, streamlining workflows, reducing administrative burdens, and improving claim accuracy. With a deep understanding of mental health billing services, we provide technology-driven solutions that enhance efficiency and maximize reimbursements. Features include:
- Automated charge capture to prevent missed billing opportunities and ensure accurate claim submissions
- Custom reporting dashboards for real-time financial tracking and revenue insights
- Integrated eligibility verification to minimize denials and prevent reimbursement delays
- HIPAA-compliant electronic claims submission for faster, more secure payment processing
With PGM’s advanced behavioral health billing technology, mental health providers can improve operational efficiency while focusing on client care.
Full Reimbursement for Mental Health Providers
PGM’s mental health billing services prioritize revenue optimization through accurate claims submission, correct coding, and proactive denial management. Our expert team ensures:
- Proper coding for mental health services, including therapy sessions, psychological assessments, and medication management.
- Accurate documentation to support medical necessity and drive down the risk of denials.
- Appeal management for denied claims to recover lost revenue.
- Negotiation with payers to secure better, fairer reimbursement rates for billing for behavioral health services.
With PGM’s behavioral health billing solutions, your practice will benefit from increased revenue, faster payments, and reduced administrative stress.
Dedicated Support for Mental Health Revenue Cycle Success
At PGM, we deliver mental health billing services with a strong emphasis on expert support, helping providers streamline operations and grow their revenue. We’ve earned a reputation as one of the top mental health billing companies because our team offers personalized guidance, proactive problem-solving, and real-time assistance to navigate billing for mental health services, evolving payer requirements, and compliance regulations. From managing strict documentation requirements to handling prior authorizations, we provide tailored solutions to minimize administrative burdens and improve cash flow.
With PGM as your billing partner, you can focus on ensuring quality care while we handle financial complexities, ensuring timely reimbursements and optimized revenue. Experience the difference of a behavioral health billing team committed to your success and long-term stability.

A Hands-On Approach to Client Support
We assign dedicated account managers who understand the unique challenges of mental health billing, ensuring smooth communication and quick issue resolution. Our team collaborates with your staff to enhance efficiency in billing for behavioral health services, cutting denials and improving cash flow. Choosing PGM means gaining more than a billing provider — you gain a committed financial partner.
Industry-Leading Mental Health Billing Expertise
PGM’s specialists are experts in mental health billing codes and payer regulations, ensuring accurate claims submission and full compliance. Whether billing for therapy sessions, psychiatric evaluations, or medication management, we ensure proper documentation and coding to reduce claim denials and enhance reimbursements. Our in-depth knowledge of behavioral health billing helps practices maintain viability and grow their revenue.
Faster, More Reliable Claims Processing
At the heart of our mental health billing services is an efficient claims management system. We take a proactive approach to reviewing claims, preventing denials, and resolving issues swiftly. Our attention to detail increases clean claim rates, improves cash flow, and reduces administrative burdens, ultimately contributing to your financial success.
Ensuring Compliance and Reducing Risk
Keeping up with Medicare, Medicaid, and private payer policies is essential for mental health providers. PGM’s experts continuously monitor regulatory changes to ensure your practice stays aligned with evolving requirements, avoiding costly penalties and delays. Our compliance-first approach ensures your mental health billing remains accurate, secure, and legally sound.
Stronger Financial Health for Your Practice
With PGM as your behavioral health billing partner, you benefit from seamless claim management, expert financial guidance, and optimized behavioral health revenue cycle management. Our commitment to accuracy and efficiency helps increase reimbursements while reducing administrative stress — so you can focus on what matters most: providing exceptional care and support to your clients.
Learn More About PGM’s Mental Health Billing Services
Are you ready to enhance your practice’s financial health? PGM offers a free consultation to explain how our expert mental health billing services improve revenue cycle management and reimbursement success.








